Discover medications that cause hair loss, including chemotherapy and antidepressants. Learn about types, treatments, and prevention for drug-induced alopecia.
Hair loss affects millions worldwide, impacting self-esteem and quality of life. While genetics and aging are common culprits, certain medications can also trigger hair loss, known as drug-induced alopecia. This condition often manifests as diffuse, nonscarring hair loss, affecting the scalp, eyebrows, or other body hair. The good news? In most cases, hair loss from medications is reversible once the drug is discontinued or adjusted. This article delves into the medications linked to hair loss, the science behind it, and practical solutions to manage or prevent it.
How Medications Cause Hair Loss
Hair growth occurs in three phases: anagen (growth, lasting 2–7 years), catagen (transitional, lasting about 10 days), and telogen (resting, lasting around 3 months). At the end of the telogen phase, hair naturally sheds, with the average person losing 100–150 hairs daily. Medications can disrupt this cycle, leading to two primary types of hair loss:
- Telogen Effluvium: The most common form of drug-induced hair loss, where medications push hair follicles prematurely into the resting phase, causing increased shedding (30–70% more than normal). Symptoms typically appear 2–4 months after starting the drug.
- Anagen Effluvium: This occurs during the growth phase, preventing hair matrix cells from dividing properly. It’s most associated with chemotherapy and results in rapid, severe hair loss, often within days to weeks.
The severity of hair loss depends on the drug type, dosage, and individual sensitivity. Below, we explore the main categories of medications linked to hair loss.
Medications That Cause Hair Loss
Numerous drugs across various therapeutic classes are associated with hair loss. Below is a detailed breakdown of the most common culprits, their mechanisms, and reported prevalence where available.
1. Chemotherapy Drugs
Chemotherapy drugs target rapidly dividing cells, such as cancer cells, but they also affect healthy cells like those in hair follicles, leading to anagen effluvium. Hair loss typically begins within 2–4 weeks of treatment and peaks after 1–2 months. According to the American Cancer Society, combination chemotherapy regimens often cause more severe hair loss than single-drug treatments. Common chemotherapy drugs linked to hair loss include:
- Cyclophosphamide (Cytoxan): Used for breast cancer and lymphomas.
- Doxorubicin (Adriamycin): Common in breast and lung cancer treatments.
- Paclitaxel (Taxol): Often used for ovarian and breast cancer.
- Docetaxel: Associated with significant hair loss in breast cancer patients.
- Etoposide, Daunorubicin, Irinotecan, Fluorouracil, Methotrexate, Nitrosoureas, Topotecan, Vinorelbine: Vary in their impact but frequently cause hair loss.
Prevalence: Up to 65% of chemotherapy patients experience hair loss, with severity varying by drug and regimen.
2. Retinoids (Vitamin A Derivatives)
Retinoids, used for acne and skin conditions, are derived from vitamin A and can cause telogen effluvium. Oral retinoids like isotretinoin (Absorica, Accutane) are particularly linked to hair shedding, especially at higher doses. Hair loss often reverses after completing the typical 15–20-week treatment course.
Prevalence: Studies suggest 10–15% of isotretinoin users experience noticeable hair loss.
3. Antidepressants
Antidepressants, used for depression, anxiety, and other mood disorders, may trigger telogen effluvium by affecting brain chemistry or hormonal balance. Commonly implicated antidepressants include:
- Bupropion (Wellbutrin): Higher risk compared to other antidepressants, with studies reporting hair loss in up to 5% of users.
- SSRIs (e.g., Fluoxetine/Prozac, Sertraline/Zoloft, Paroxetine/Paxil, Fluvoxamine/Luvox): Hair loss may occur after 8–12 weeks.
- SNRIs (e.g., Duloxetine/Cymbalta, Venlafaxine/Effexor): Less common but reported.
Prevalence: A 2022 review found that 63% of SSRI-related hair loss cases resolved after discontinuation.
4. Anticoagulants (Blood Thinners)
Anticoagulants prevent blood clots but can cause telogen effluvium in some users. The exact mechanism is unclear, but it may involve disruption of follicular nutrient supply. Common anticoagulants include:
- Heparin: Often linked to hair loss within weeks.
- Warfarin (Coumadin, Jantoven): May cause shedding months to years after starting.
- Apixaban (Eliquis), Rivaroxaban (Xarelto): Newer anticoagulants with occasional reports of hair loss.
Prevalence: Hair loss is reported in less than 5% of anticoagulant users.
5. Anticonvulsants
Anticonvulsants, used for epilepsy and mood disorders, stabilize brain activity but may disrupt hair growth. Drugs with higher risk include:
- Valproic Acid (Depakote): Hair loss in 12–28% of users, dose-dependent.
- Lamotrigine (Lamictal): Linked to hair loss in some case reports.
- Carbamazepine (Tegretol): Up to 6% prevalence.
Prevalence: Varies widely, with valproic acid being the most significant contributor.
6. Beta-Blockers
Beta-blockers, used for hypertension and heart conditions, rarely cause telogen effluvium. Common examples include:
- Propranolol (Inderal), Atenolol (Tenormin), Metoprolol (Lopressor): Hair loss is uncommon, affecting less than 2% of users.
7. Antithyroid Medications
Antithyroid drugs like methimazole (Tapazole) and propylthiouracil, used for hyperthyroidism, can exacerbate hair loss already caused by thyroid imbalances. Hair loss is typically telogen effluvium and reversible with dose adjustment or thyroid stabilization.
Prevalence: Approximately 5–10% of users report hair loss.
8. Hormone Therapies
Hormonal medications, including birth control pills, hormone replacement therapy (HRT), and testosterone replacement therapy (TRT), can disrupt hair growth by altering estrogen or androgen levels. Tamoxifen, used for breast cancer, blocks estrogen receptors, leading to hair thinning in some patients.
Prevalence: Hair loss occurs in 5–10% of tamoxifen users and varies with hormonal therapies.
9. Arthritis Medications
Disease-modifying antirheumatic drugs (DMARDs) like methotrexate (up to 3% prevalence) and leflunomide (Arava) (up to 10% prevalence) can slow hair growth, causing telogen effluvium. Biologic DMARDs like etanercept (Enbrel) and adalimumab (Humira) rarely cause hair loss.
10. Weight Loss Drugs
Semaglutide medications (Ozempic, Wegovy) are associated with hair loss, potentially due to rapid weight loss rather than the drug itself. Weight loss can trigger telogen effluvium by stressing the body or causing nutrient deficiencies.
Prevalence: Reported in less than 5% of users, often linked to weight loss rather than the drug.
11. Other Medications
- Allopurinol (Zyloprim): Used for gout, with rare case reports of hair loss.
- Levodopa (Sinemet): For Parkinson’s disease, may inhibit hair growth via dopamine-like effects.
- Antifungals (e.g., Fluconazole): Linked to telogen effluvium in recent studies.
- NSAIDs (e.g., Naproxen): Rarely cause hair loss.
- Monoclonal Antibodies (e.g., Infliximab, Dupilumab): May cause telogen effluvium or alopecia areata.
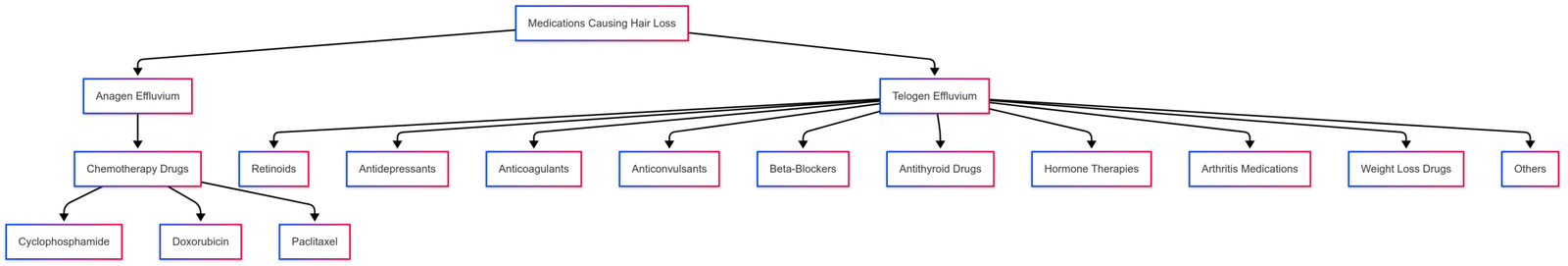
Visualizing Medication-Related Hair Loss
The following Mermaid chart categorizes medications by their likelihood of causing hair loss and the type of alopecia they induce.
Diagnosis of Drug-Induced Alopecia
Diagnosing drug-induced hair loss involves a systematic approach to rule out other causes and confirm the medication’s role. Key steps include:
- Medical History: A detailed history of medications (including over-the-counter drugs and supplements) taken in the three months before hair loss began. Other factors like recent illness, surgery, or family history of androgenetic alopecia are also considered.
- Scalp Examination: Assessing the degree and pattern of hair loss, checking for redness, scaling, or hair shaft abnormalities.
- Hair Pull Test: Gently pulling a cluster of hairs to count shedding (normal: 1–2 hairs; abnormal: 10–15 hairs). Microscopic analysis identifies anagen or telogen bulbs.
- Scalp Biopsy: Rarely needed, but useful to exclude conditions like alopecia areata or scarring alopecia.
- Blood Tests: To check for nutritional deficiencies, thyroid function, or hormonal imbalances.
The definitive test is stopping the suspected drug for at least three months to observe regrowth, but this must be done under medical supervision.
Treatment Options for Drug-Induced Hair Loss
Treating drug-induced hair loss focuses on addressing the root cause and promoting regrowth. Options include:
1. Discontinuing or Adjusting the Medication
- Primary Approach: Stopping the offending drug often reverses hair loss within 3–6 months, with full cosmetic recovery taking 12–18 months. However, discontinuation isn’t always possible (e.g., for chemotherapy or essential medications).
- Consultation: Always consult a healthcare provider before stopping or changing medications, as abrupt cessation can cause serious side effects (e.g., with antidepressants or levodopa).
2. Scalp Hypothermia for Chemotherapy
- Mechanism: Cooling caps reduce blood flow to hair follicles, limiting chemotherapy drug exposure. Worn 30 minutes before, during, and 90 minutes after treatment.
- Effectiveness: Reduces hair loss in 50–70% of patients, but carries a small risk of cancer recurrence in the scalp due to reduced drug delivery.
- Cost: Cooling cap sessions typically cost $100–$500 per treatment, depending on the provider and region.
3. Topical Treatments
- Minoxidil (Rogaine): A topical solution (2% or 5%) that stimulates hair follicles and promotes regrowth. Effective for telogen effluvium and post-chemotherapy regrowth. Cost: $15–$50 for a 2-month supply.
- Note: Minoxidil may not work for all medication-induced hair loss, as stated on some product labels.
4. Low-Level Laser Therapy (LLLT)
- Mechanism: Devices like laser caps or combs stimulate blood flow and hair follicle activity. Brands like HairMax or Capillus are FDA-cleared for hair loss.
- Effectiveness: Studies show 20–40% improvement in hair density after 6 months of use.
- Cost: Devices range from $200 (combs) to $3,000 (helmets).
5. Nutritional Supplements
- Nutrafol: A supplement containing peptides, amino acids, and vitamins like biotin to support hair growth. Cost: $80–$100 for a 1-month supply.
- Other Nutrients: Vitamin C, omega-3 fatty acids, and iron supplements may help if deficiencies are identified.
6. Cosmetic Solutions
- Wigs and Hairpieces: Used during chemotherapy or severe hair loss to boost confidence. Cost: $50–$2,000, depending on quality.
- Scalp Micropigmentation: A tattoo-like technique to mimic hair follicles, costing $1,000–$4,000.
Treatment Comparison Table
| Treatment | Effectiveness | Cost (USD) | Best For |
|---|---|---|---|
| Scalp Hypothermia | 50–70% reduction | $100–$500/session | Chemotherapy patients |
| Minoxidil (Rogaine) | 30–60% regrowth | $15–$50/2 months | Telogen effluvium, post-chemo |
| Low-Level Laser Therapy | 20–40% density increase | $200–$3,000 (device) | Chronic hair loss |
| Nutrafol Supplement | Varies, nutrient-based | $80–$100/month | Nutrient deficiency-related loss |
| Wigs/Hairpieces | Cosmetic solution | $50–$2,000 | Temporary coverage |
Prevention Strategies
Preventing drug-induced hair loss involves proactive steps, especially for high-risk medications like chemotherapy drugs:
- Scalp Cooling: As mentioned, cooling caps can significantly reduce hair loss during chemotherapy.
- Gentle Hair Care: Use mild shampoos, avoid heat styling, and use silk pillowcases or microfiber towels to reduce hair breakage.
- Nutritional Support: Ensure adequate intake of protein, iron, and vitamins (e.g., biotin, vitamin D) to support hair health.
- Regular Monitoring: Discuss potential side effects with your doctor before starting a new medication, and monitor for early signs of shedding.
Real-Life Experiences
Personal stories highlight the emotional toll of drug-induced hair loss. For example, a user on a social platform shared their struggle with hair loss while on lamotrigine (Lamictal), a mood stabilizer. Despite its effectiveness for anxiety, they noticed significant thinning after three years, leading to reduced confidence. Attempts with rosemary oil and minoxidil foam were ineffective, and reducing the dose to 50 mg caused mental health challenges without improving hair loss. Another user reported losing a quarter of their hair volume after starting methotrexate and leflunomide for rheumatoid arthritis, underscoring the need for medical guidance to explore alternatives.
Frequently Asked Questions
What drugs are most likely to cause hair loss?
Chemotherapy drugs (e.g., cyclophosphamide, doxorubicin), retinoids (e.g., isotretinoin), antidepressants (e.g., bupropion), and anticonvulsants (e.g., valproic acid) are among the most common culprits.
How can I tell if my medication is causing hair loss?
Look for increased shedding (e.g., in hairbrushes or shower drains) or thinning within 2–4 months of starting a new drug. Consult a doctor for a hair pull test or scalp analysis.
Can hair loss from medications be permanent?
In rare cases, particularly with prolonged use of certain drugs (e.g., tamoxifen), hair loss may persist. However, most cases are reversible upon discontinuation.
How can I prevent hair loss while on medication?
Use scalp cooling for chemotherapy, maintain a nutrient-rich diet, and discuss lower-risk medication alternatives with your doctor.
The Bottom Line
Drug-induced hair loss, whether from chemotherapy, antidepressants, or other medications, can be a challenging side effect, but it’s often reversible. By understanding the medications involved, recognizing early signs, and exploring treatments like minoxidil or scalp hypothermia, you can manage or mitigate hair loss effectively. Always consult a healthcare provider before making changes to your medication regimen, as they can recommend alternatives or treatments tailored to your needs. With the right approach, you can protect your hair and maintain confidence during treatment.
Please share this Medications & Drugs That Cause Hair Loss with your friends and do a comment below about your feedback.
We will meet you on next article.
Until you can read, Hairmax LaserBand Review: Does It Really Work?
