Discover alopecia areata: its types, causes, diagnosis, and treatments. Learn about effective therapies and management strategies for this autoimmune hair loss condition.
Alopecia areata is an autoimmune condition that causes unpredictable, patchy hair loss, primarily affecting the scalp but potentially impacting any hair-bearing area of the body. With nearly 7 million people affected in the United States alone, according to the National Alopecia Areata Foundation (NAAF), it ranks as the second-most common form of hair loss after pattern baldness. This article provides an in-depth exploration of alopecia areata, covering its types, causes, symptoms, diagnosis, and treatment options, alongside practical strategies for living with the condition.
Understanding Alopecia Areata
Alopecia areata occurs when the immune system mistakenly attacks hair follicles, leading to hair loss in small, round patches about the size of a quarter. The term “alopecia” refers to hair loss, while “areata” indicates its patchy nature. The condition can manifest in various forms, ranging from mild, localized hair loss to complete scalp or body hair loss. Its unpredictable course makes it a challenging condition for both patients and healthcare providers.
Types of Alopecia Areata
The presentation of alopecia areata varies, and its classification depends on the extent and pattern of hair loss:
- Patchy Alopecia Areata: The most common form, characterized by one or more coin-sized bald patches on the scalp or body.
- Alopecia Totalis: Complete loss of scalp hair, affecting up to 5% of patients.
- Alopecia Universalis: Loss of all hair on the scalp and body, a rare form affecting less than 1% of patients.
- Diffuse Alopecia Areata (Alopecia Areata Incognita): Widespread thinning across the scalp, resembling pattern hair loss.
- Ophiasis Alopecia Areata: A band-like pattern of hair loss along the lower back and sides of the scalp.
- Sisaipho (Ophiasis Inversus): Hair loss on the frontal, temporal, and parietal scalp, mimicking male pattern baldness.
Each type presents unique challenges, with more extensive forms like totalis and universalis often being harder to treat.
Prevalence and Risk Factors
Alopecia areata affects approximately 2% of the population over their lifetime, with a peak incidence in the second and third decades of life. It occurs across all genders, ethnicities, and skin types, though certain factors increase the risk:
- Genetics: A family history of alopecia areata significantly raises the likelihood of developing the condition. At least 16 genetic risk loci, including human leukocyte antigen (HLA) alleles, have been identified.
- Autoimmune Conditions: Individuals with conditions like thyroid disease, vitiligo, or Down syndrome are at higher risk.
- Age: Children and young adults are more commonly affected, with early onset often linked to more severe cases.
- Nutritional Deficiencies: Low levels of vitamin D, zinc, iron, or biotin may contribute to hair loss.
Notably, Black and Hispanic females may have a higher incidence of alopecia areata compared to white females, based on studies like the Nurses’ Health Study, though further research is needed to understand these disparities fully.
Causes of Alopecia Areata
Alopecia areata is driven by an autoimmune response where the immune system targets hair follicles, mistaking them for foreign invaders. This attack disrupts the hair growth cycle, particularly the anagen (growth) phase, causing follicles to enter the telogen (resting) phase prematurely, leading to hair loss.
Immune Privilege Hypothesis
Healthy hair follicles typically enjoy “immune privilege,” a state that shields them from immune surveillance. In alopecia areata, this privilege is lost, allowing autoreactive CD8+ T cells to attack hair follicle autoantigens. Histopathological studies show a dense T-cell infiltrate around anagen follicles, a hallmark of active disease.
Genetic and Environmental Triggers
The condition has a strong hereditary component, with complex inheritance patterns influenced by environmental factors. Potential triggers include:
- Stress: While not definitively proven, emotional or physiological stress is often reported before the onset of hair loss.
- Viral or Environmental Factors: These may interact with genetic predispositions to initiate the autoimmune response.
- Medications: Nivolumab, a cancer drug, can induce alopecia areata as a side effect, signaling its immune-modulating activity.
Symptoms of Alopecia Areata
The hallmark symptom is patchy hair loss, typically on the scalp, but it can affect the beard, eyebrows, eyelashes, or other body hair. Other symptoms include:
- Nail Changes: Pitting, ridging, or brittleness, seen in 10–40% of patients, particularly those with severe disease.
- Exclamation Point Hairs: Short, broken hairs that are thicker at the tip and taper toward the scalp.
- Trichodynia: Localized itching or tingling before hair loss.
- Regrowth Characteristics: Regrown hair may initially be white or blonde and finer, though it often returns to its original color and texture with time.
In rare cases, affected areas may itch, change color, or show visible follicular openings or black dots (cadaver hairs).
Diagnosis of Alopecia Areata
Diagnosing alopecia areata typically begins with a clinical evaluation by a dermatologist, who specializes in hair, skin, and nail conditions. The process involves:
- Physical Examination: The dermatologist inspects bald patches and nails for characteristic signs like pitting or exclamation point hairs.
- Dermoscopy: A dermatoscope, a handheld magnifying device, reveals features such as yellow dots, black dots, or dystrophic hairs.
- Medical and Family History: Questions about onset, family history of alopecia or autoimmune diseases, and other health conditions help confirm the diagnosis.
- Hair Pull Test: Gently tugging 40–60 hairs to assess fragility; a positive test (over 10% hairs easily removed) suggests active disease.
- Scalp Biopsy: If the diagnosis is unclear, a small skin sample is examined microscopically, revealing a “bee-swarm” pattern of lymphocytic infiltrates around follicles.
- Blood Tests: These screen for associated conditions like thyroid disease or iron deficiency.
The Severity of Alopecia Areata Lesion Tool (SALT) score quantifies scalp hair loss, with SALT 50 indicating 50% scalp involvement. A SALT score of 40 or higher is considered severe. The Alopecia Areata Severity and Morbidity Index (ASAMI) also considers eyebrow/lash loss and psychosocial impact.
Differential Diagnosis
Other conditions mimicking alopecia areata include:
- Trichotillomania: Hair loss from compulsive pulling.
- Tinea Capitis: Fungal scalp infection.
- Telogen Effluvium: Diffuse hair shedding due to stress or hormonal changes.
- Androgenetic Alopecia: Pattern hair loss in males or females.
- Lichen Planopilaris: Scarring alopecia with inflammation.
Accurate diagnosis is critical to avoid ineffective treatments.
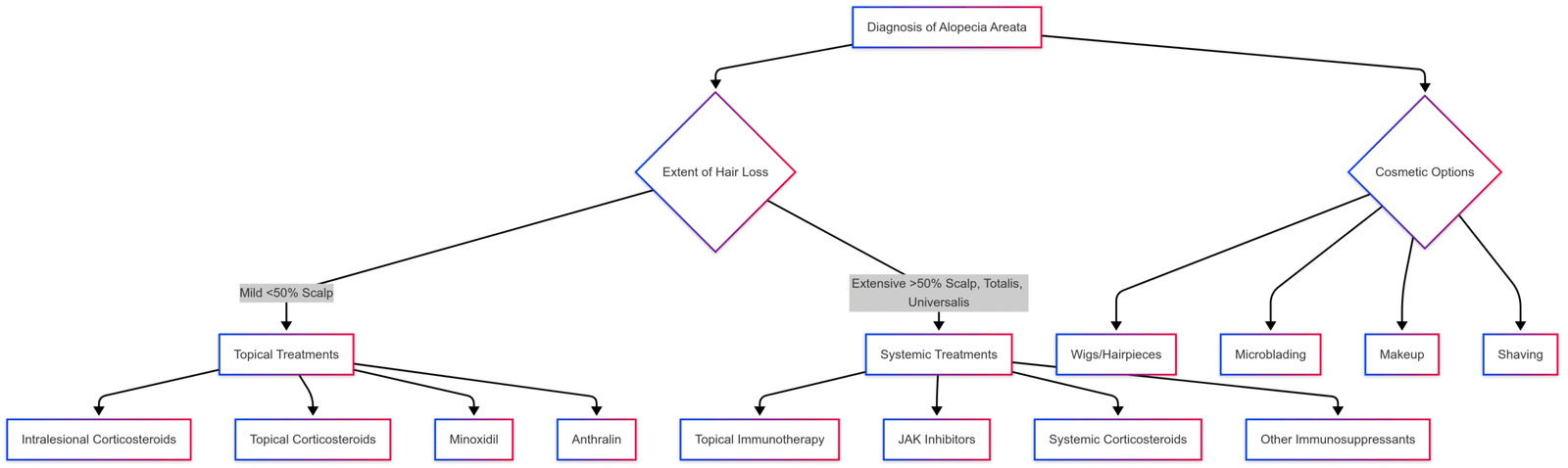
Treatment Options for Alopecia Areata
There is no cure for alopecia areata, but treatments aim to suppress the immune attack on hair follicles and stimulate regrowth. Treatment choice depends on the patient’s age, extent of hair loss, and preferences. Some opt for no treatment, especially in mild cases where spontaneous regrowth is common.
Treatments for Mild Alopecia Areata (Less Than 50% Scalp Involvement)
Intralesional Corticosteroids:
- Description: Triamcinolone injections into bald patches suppress local inflammation.
- Effectiveness: Over 80% of patients with patchy hair loss see at least 50% regrowth within 12 weeks.
- Administration: Injected every 4–6 weeks; typically used in adults due to pain.
- Side Effects: Temporary skin atrophy or discomfort at injection sites.
Topical Corticosteroids:
- Description: Potent creams or lotions (e.g., clobetasol) applied to bald spots.
- Effectiveness: More effective in children; often combined with occlusive dressings.
- Side Effects: Skin thinning or irritation with prolonged use.
Minoxidil (Rogaine®):
- Description: A topical solution applied 2–3 times daily to maintain regrowth.
- Effectiveness: Best used after corticosteroids to sustain results; limited efficacy alone.
- Side Effects: Scalp irritation or unwanted facial hair growth.
Anthralin:
- Description: A topical irritant applied for a set time, then washed off.
- Effectiveness: Induces mild irritation to stimulate regrowth; used with minoxidil.
- Side Effects: Skin staining or irritation, limiting use in light-haired individuals.
Treatments for Extensive Alopecia Areata (Over 50% Scalp Involvement, Totalis, or Universalis)
Topical Immunotherapy:
- Description: Chemicals like diphenylcyclopropenone (DPCP) are applied weekly to induce a controlled allergic reaction, diverting immune activity from follicles.
- Effectiveness: Regrowth rates range from 17–75%; requires consistent weekly treatments.
- Side Effects: Severe dermatitis, lymph node swelling, or skin discoloration.
- Process: A small amount is applied initially to sensitize the skin, followed by weekly applications left on for 48 hours.
Janus Kinase (JAK) Inhibitors:
- Description: Oral medications that block inflammatory cytokines, calming the immune response.
- Approved Drugs:
- Baricitinib: FDA-approved for adults with severe alopecia areata; taken once daily. Price: Approximately $2,500–$3,000/month (varies by insurance).
- Deuruxolitinib: FDA-approved for adults; taken twice daily. Price: Estimated $2,000–$2,800/month.
- Ritlecitinib: FDA-approved for adults and children 12+ with extensive hair loss; taken once daily. Price: Around $2,400–$3,200/month.
- Effectiveness: Up to 40% of patients achieve a SALT score of 20 or less after one year.
- Side Effects: Increased infection risk, liver enzyme elevation, or blood clots.
- Note: Long-term safety and outcomes after discontinuation are under study.
Systemic Corticosteroids:
- Description: Oral prednisone or similar drugs for short-term use in severe cases.
- Effectiveness: Can induce regrowth but limited by side effects.
- Side Effects: Weight gain, mood changes, high blood pressure, or bone loss.
Other Systemic Treatments:
- Methotrexate or Cyclosporine: Immunosuppressants for refractory cases; long-term use is risky due to liver/kidney damage or infection risk.
- Emerging Therapies: Dupilumab, platelet-rich plasma, or micro-needling show promise but lack robust evidence.
Treatments for Eyebrow and Eyelash Loss
- Intralesional Corticosteroids: Injections to stimulate eyebrow regrowth, often followed by minoxidil.
- JAK Inhibitors: Effective for significant eyebrow/eyelash loss, with studies showing noticeable regrowth.
- Bimatoprost: A glaucoma drug applied to eyelashes to promote lengthening; off-label for alopecia areata.
- Cosmetic Solutions: Artificial eyelashes (individual, clusters, or strips) or microblading for eyebrows.
Treatments for Nail Changes
Nail pitting or brittleness can be distressing. Options include:
- Topical Treatments: Corticosteroids or tazarotene applied to nails.
- Injections: Corticosteroid injections into affected nails (adults only).
- Observation: In children, nail changes may resolve without treatment.
Non-Medical and Cosmetic Options
For those avoiding medical treatments or seeking camouflage, options include:
- Wigs and Hairpieces: Custom scalp prostheses or wigs (e.g., vacuum wigs, $1,000–$3,000) provide a natural look.
- Styling Products: Gels, mousses, or powders add volume and coverage.
- Shaving: Eliminates patchy appearance for a uniform look.
- Microblading: Semi-permanent eyebrow pigmentation ($300–$800 per session).
- Makeup: Eyebrow pencils or waterproof eyeliner for daily camouflage.
Treatment Decision Flowchart
Living with Alopecia Areata
Alopecia areata does not cause physical disability but can profoundly affect mental health, leading to stress, anxiety, or depression. Strategies to cope include:
- Support Networks: Joining groups like the NAAF connects patients with others facing similar challenges.
- Mental Health Support: Counseling addresses emotional distress and boosts self-confidence.
- Protective Measures:
- Use sunscreen on exposed scalp areas.
- Wear hats, scarves, or wigs to shield the scalp from sun and cold.
- Use glasses or sunglasses to protect eyes if eyelashes are lost.
- Healthy Lifestyle: A Mediterranean diet rich in fruits, vegetables, and lean proteins may support hair health. Vitamin D supplements could help, though evidence is limited.
Regular check-ups with a primary care physician are crucial, as alopecia areata is associated with a higher risk of thyroid disease, eczema, or other autoimmune conditions.
Prognosis and Outlook
The course of alopecia areata is unpredictable. Mild cases often see spontaneous regrowth within a year, especially in children. However, relapses are common, with many experiencing recurrent hair loss within five years. Extensive forms like totalis or universalis have a lower likelihood of regrowth, with a 5–10% risk of progression from patchy to total hair loss.
Factors predicting poorer outcomes include:
- Early onset (before age 10)
- Extensive hair loss
- Prolonged hair loss (over one year)
- Nail dystrophy
- Ophiasis pattern
- Family history or coexisting autoimmune diseases
Despite these challenges, advancements in treatments like JAK inhibitors offer hope, with some patients achieving significant regrowth.
Frequently Asked Questions
What causes alopecia areata?
It’s an autoimmune condition triggered by genetic, environmental, or stress-related factors, with no single known cause.
Is alopecia areata contagious?
No, it cannot be spread through contact or airborne particles.
Can hair grow back?
Yes, hair can regrow spontaneously or with treatment, though outcomes vary. Regrowth may take 6–12 weeks with therapy.
Is there a cure?
No cure exists, but treatments can manage symptoms and promote regrowth.
How can I prevent it?
Prevention is not possible, but early treatment and lifestyle adjustments may reduce severity.
Conclusion
Alopecia areata is a complex autoimmune condition that demands a tailored approach to diagnosis and treatment. From clinical evaluations and dermoscopy to advanced therapies like JAK inhibitors, dermatologists play a pivotal role in managing this condition. While no cure exists, a combination of medical treatments, cosmetic solutions, and emotional support can significantly improve quality of life. By staying informed and proactive, individuals with alopecia areata can navigate its challenges with confidence and resilience.
References
- Pratt CH, King LE Jr, et al. “Alopecia areata.” Nat Rev Dis Primers. 2017;3:17011.
- Freitas E, Guttman-Yassky E, et al. “Baricitinib for the treatment of alopecia areata.” Drugs. 2023;83(9):761-70.
- King B, Zhang X, et al. “Efficacy and safety of ritlecitinib in alopecia areata.” The Lancet. 2023;0(0).
- Barton VR, Toussi A, et al. “Treatment of pediatric alopecia areata: A systematic review.” J Am Acad Dermatol. 2022;86(6):1318-34.
- National Alopecia Areata Foundation (NAAF).
Please share this Hair loss types: Alopecia areata diagnosis and treatment with your friends and do a comment below about your feedback.
We will meet you on next article.
Until you can read, Toppik Hair Fiber Review – Cheap and effective concealer
